The Comprehensive Guide to Heart Palpitations
2. Causes of Heart Palpitations
3. How the Heart Works
4. Are Heart Palpitations Dangerous?
5. What to Tell Your Doctor
6. Diagnosis
First, some good news: heart palpitations in healthy hearts are generally considered to be completely benign. Palpitations are a common condition and in most cases can be controlled with basic lifestyle changes and nutritional intervention. However, if you have never experienced heart palpitations before, if they have changed in frequency or severity, or if you have any concerns regarding the health of your heart you should consult your doctor.
What are heart palpitations?
Heart palpitations are an intense awareness of your heartbeat, caused by a feeling that your heart is beating too quickly, slowly, forcefully, or irregularly. The sensation is frequently described as feeling like your heart is skipping a beat or flip-flopping in your chest. In some cases, palpitations manifest themselves as a feeling of anxiety or unease.
The frequency and severity of heart palpitations can vary widely. They may last for a few seconds, several minutes or hours, or even days. It is possible to have a single episode, occasional episodes, or frequent episodes depending on the cause or trigger.
In the most fundamental sense, heart palpitations are caused by changes to the electrical system that controls the heart. Heart palpitations are generally not directly related to circulation problems although in extreme cases, slow, irregular, or less efficient heartbeats can have a broad impact on the cardiovascular system. This is why you should consult your doctor when you first experience heart palpitations.
Some people only experience heart palpitations when they are lying down. In most cases, they have palpitations while they are awake and upright, but they do not notice them until they are preparing for sleep or are in a calm, quiet environment.
Heart palpitations are frequently caused by stress or anxiety. In addition to making you feel terrible emotionally, stress can have a physical effect on your body. As a result, stress can cause the nerve endings that control your heart to fire more frequently or irregularly. Anxiety and panic attacks can also trigger palpitations by elevating adrenaline levels.
Food and drink can cause heart palpitations. Caffeine, nicotine, and alcohol can all affect your heart rate and may also increase the likelihood of irregular heartbeats.
Underlying health issues can trigger heart palpitations. Fevers, dehydration, thyroid problems, low blood sugar, low blood pressure and anemia can all cause irregular heartbeats, so if you are suffering from any of these conditions, they may be responsible. Hormonal changes, such as those associated with the menstrual cycle or menopause may also cause periodic palpitations.
The act of lying down can also trigger heart palpitations. This may be due to activation of the vagus nerve, which is a major component of the parasympathetic nervous system and travels from your brain to your abdomen. The vagus nerve is one of the nerves responsible for controlling your heart rate. Due to the position of the vagus nerve in your body, it’s possible that lying on your back or left side can stimulate this nerve, sending an errant signal to the heart resulting in palpitations. This illustration shows the many functions of the parasympathetic nervous system and the vagus nerve.

The heart as an electrical system
Irregular heartbeats are generally caused by improper signaling within the electrical system of your heart. To better understand heart palpitations, it’s important to understand how the heart functions.
The heart is a muscle. Muscle cells contract when they receive electrical signals from other cells. In your skeletal muscles, like your biceps, the electrical signals that tell the muscle fibers to contract come from your nervous system. The muscle cells of the heart are coordinated more closely. The contraction of heart muscle cells sends an electrical message to the other nearby cells, causing the heart to beat in a controlled manner, starting with the top chambers (the atria) followed by the bottom chambers (the ventricles).
Heartbeats start at the sinus, or SA node, which is located at the top of the right atria. This bundle of muscle fibers is able to initiate the electrical signal that starts a heartbeat. The SA node is also called the heart’s pacemaker because it sets the pace of your heartbeat. Signals from the sympathetic and parasympathetic nervous systems tell the SA node to speed up or slow down, but the node itself makes sure that your heart continues to beat steadily.
During diastole, which is the stage in your heartbeat between contractions, the entire heart is relaxed and the atria fill with blood. Diastole ends when the SA node sends a message to rest of the right atrium to contract, which results in the atrial systole.
While the atria contract to send blood to the ventricles, the electrical signal travels through the atria to the AV, or atrioventricular node. This bundle of muscle fibers is located on the interatrial septum (the wall between the two atria), near the bottom of the atria. The AV node pauses the electrical signal to allow the ventricles to fill with blood from the atria.
Finally, the electrical signal travels from the AV node through the His-Purkinje system to the bottom of the ventricles, where it sets off the ventricular systole. This pumps blood out of the ventricles into the lungs and the rest of the body.
Are heart palpitations dangerous?
Most heart palpitations are not symptoms of an underlying illness and are not considered dangerous at all. However, if this is a new symptom for you, or your palpitations increase in frequency or strength, you should consult your doctor.
Some symptoms including dizziness, nausea, chest pain, shortness of breath, upper back, arm, or jaw pain, or intense pressure in the chest can be indicative of a much more serious condition including a heart attack and require immediate medical attention.
Even though heart palpitations are typically benign, you should check with your doctor to make sure that this is the case for you. You should also visit your doctor if your palpitations change in frequency or the sensation changes.
There are several things that your doctor will want to know in order to decide which tests are necessary to make a correct diagnosis. If you are able to do so, you should keep track of how long your episodes of heart palpitations last, how often they occur, when you first experienced them, and if there are any specific behaviors that may trigger these palpitations.
Your doctor will also need to know about any changes in your diet or lifestyle, especially those that cause stress or anxiety.
It is also important to make sure that your doctor has access to any potentially related health information like your history of heart health, and any other symptoms that you may have experienced with the palpitations, like shortness of breath, chest pain, nausea, or faintness.
How are heart palpitations diagnosed?
There are several methods available to measure the beating of your heart depending on the severity of the problem and the length of time that the measurement needs to take place. The measurements that your doctor will want to do will depend on the general health of your heart, your medical history, and the nature of your heart palpitations. These measurements, combined with the symptoms that you report to your doctor, will allow your doctor to diagnose your heart palpitations or any underlying illnesses that cause them.
The first method for monitoring your heartbeat is called an EKG, or ECG, which stands for electrocardiogram. This method tracks the beating of your heart by measuring the electrical signals that the different parts of your heart send out. As mentioned earlier, every step of your heartbeat is caused by the muscle cells in your heart sending electrical signals to each other.
The EKG pattern is a series of peaks, named PQRST. This is the measured signal that you often see on monitors in hospital scenes in television shows or movies. Although the EKG will probably not detect your actual heart palpitations, your doctor can use it to make sure that you are not suffering from an obvious arrhythmia. EKGs are completely painless and only take a few seconds to perform.
An EKG can be followed up with a different type of diagnostic test, called an echocardiogram, which takes an image of your heart so that your doctor can check for structural problems. Echocardiograms use ultrasound waves and form an image of your heart based on the “echoes” as the sound waves bounce back.
The echocardiogram is typically done at the same time as another EKG measurement so that your doctor can compare the visual information about what the structure of your heart is doing with the electrical signals that it is sending off.
An echocardiogram can also be combined with a stress test to get a better idea of how your heart beats while you’re stressed out or exercising.

Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Service
The stress test is a method to diagnose heart problems that may only show up when you’re exercising or your heart is otherwise working harder than it does when you’re resting. The stress test may also be called an exercise or treadmill test.
A standard stress test will require you to exercise for a few minutes so that your heart starts to work harder. Your doctor will tell you what your target heart rate is based on your age and health, so you can exercise until you reach that point.
However, you should not exercise harder than you feel you are able, and should inform the doctor performing the stress test if you feel that you cannot continue. Other reasons to stop a stress test early include: your heart begins to beat irregularly, you feel out of breath, you experience chest pain, or your blood pressure changes drastically.
During a stress test, both your EKG (the electrical activity of your heart) and blood pressure are monitored continuously. In some stress tests, typically called echo stress tests, an echocardiogram of your heart is taken after you have reached the target heart rate.
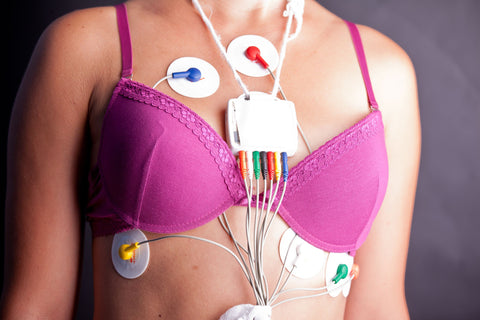
The Holter monitor is a small, wearable heart monitor that keeps track of your heartbeat throughout the entire day. The length of time that you will be expected to wear it depends on how long your doctor wants to monitor you. The benefit of the Holter monitor is that it will record a measurement of your heart’s electrical activity while you go about your daily activities and can give a more accurate picture than what may be gained through tests done in the doctor’s office.
Wearing a Holter monitor does not come with any real risks. However, while wearing a Holter monitor, it’s important to remember that it is measuring electrical signals. Therefore, you should avoid situations in which you will be subjected to strong electrical or magnetic fields. Thus, your cell phone should not be placed near the monitor, and you should avoid going through metal detectors. The Holter monitor should also never get wet, so you will have to forgo bathing or swimming while you are wearing it.
If a one or two day Holter test is not enough for your doctor to get a full picture of what is happening with your heart, he or she may suggest that you do a longer test, which can require wearing a monitor for 30 days or longer. These longer-term monitors, often referred to as event monitors, can be more easily removed to facilitate bathing and may have different features than a standard Holter monitor.
What can you do to control or stop heart palpitations on your own?
In many cases, the heart palpitations caused by stress or anxiety can be controlled with basic lifestyle changes. For example, cutting back on drugs that can trigger palpitations, like alcohol, caffeine, and other stimulants can help. Getting proper sleep can also help, so if you have difficulty sleeping, look into improving your sleep quality.
One of the most important things to remember when experiencing these symptoms is not to panic, especially if your palpitations are triggered by strong emotions or anxiety. Panic can trigger more palpitations or cause the symptoms to last longer than they ordinarily would. Relaxation techniques can help reduce the time you spend dealing with heart palpitations.
Deep Breathing for Immediate Relaxation
Deep breathing can be a wonderful way to quickly calm down and reduce palpitations. One of our favorite techniques is called 4-7-8 breathing. The method is as follows:
- Breathe through your nose for 4 seconds
- Hold your breath for 7 seconds
- Release your breath through your mouth while making a “wooshing” sound for 8 seconds
- Repeat cycle
The 4-7-8 breathing cycle should repeated 3-5 times. In just a couple of minutes you should feel yourself starting to relax.
Exercise for better heart health
Exercise might sound counter-intuitive when it comes to heart palpitations, but it can actually be quite helpful for reducing their occurrence. Exercise, particularly cardiovascular exercises like jogging or biking, can be a great way to strengthen your heart muscle and make it beat more efficiently. Exercise is also a great way to strengthen the parasympathetic nervous system and reduce excessive adrenaline release. The parasympathetic nervous system is responsible for calming the body and heart down.
Heart palpitations may be a result of an electrolyte imbalance. Although you typically don’t see electrolytes discussed outside of advertisements for sports drinks, they are important elements that your body needs to function.
Common electrolytes include sodium, potassium, magnesium. These elements form positively charged ions inside of your body. The ability of your heart to regulate its contractions is related to the movement of these ions across the membranes of your heart cells.
Coenzyme Q10, or CoQ10 is an important antioxidant that your cells use to produce energy. Your heart needs CoQ10 to continue beating steadily, and to allow your SA node to produce its pacemaker rhythm. CoQ10 is depleted by some blood pressure medications, so if you are also being treated for high blood pressure, CoQ10 may be an essential supplement.
Taurine is another supplement that can help maintain heart health. Taurine is an important amino acid that regulates levels of calcium, potassium, sodium and magnesium within the heart. Taurine can also help to prevent feelings of stress and anxiety by reducing elevated levels of adrenaline with the body.
While each of these nutrients is important on its own, when taken together they can potentially lead to a significant improvement in the severity and frequency of heart palpitations.
Just remember, don't panic!
Benign heart palpitations can be frightening, but with this knowledge on your side and a thorough examination from your doctor, you should feel confident in your ability to face them. In most cases, you will be able to reduce your heart palpitations without significant intervention. If you experience heart palpitations, take a deep breath, try to relax, and work on taking the steps necessary to improve your heart health.